
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- Basic Research
- Notch1 Has an Important Role in β-Cell Mass Determination and Development of Diabetes
- Young Sil Eom, A-Ryeong Gwon, Kyung Min Kwak, Jin-Young Youn, Heekyoung Park, Kwang-Won Kim, Byung-Joon Kim
- Diabetes Metab J. 2021;45(1):86-96. Published online February 26, 2020
- DOI: https://doi.org/10.4093/dmj.2019.0160
- 6,338 View
- 185 Download
- 7 Web of Science
- 6 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub 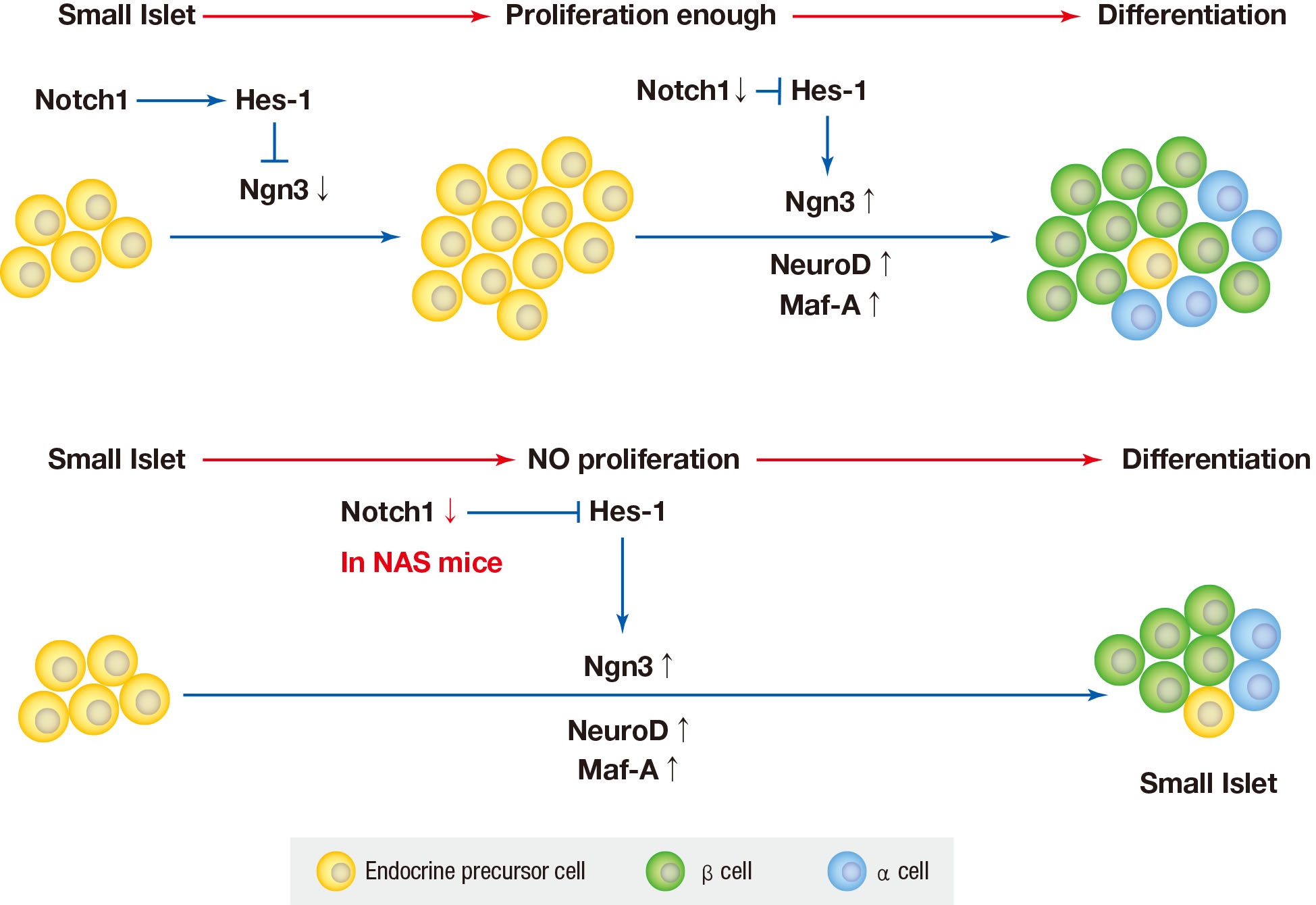
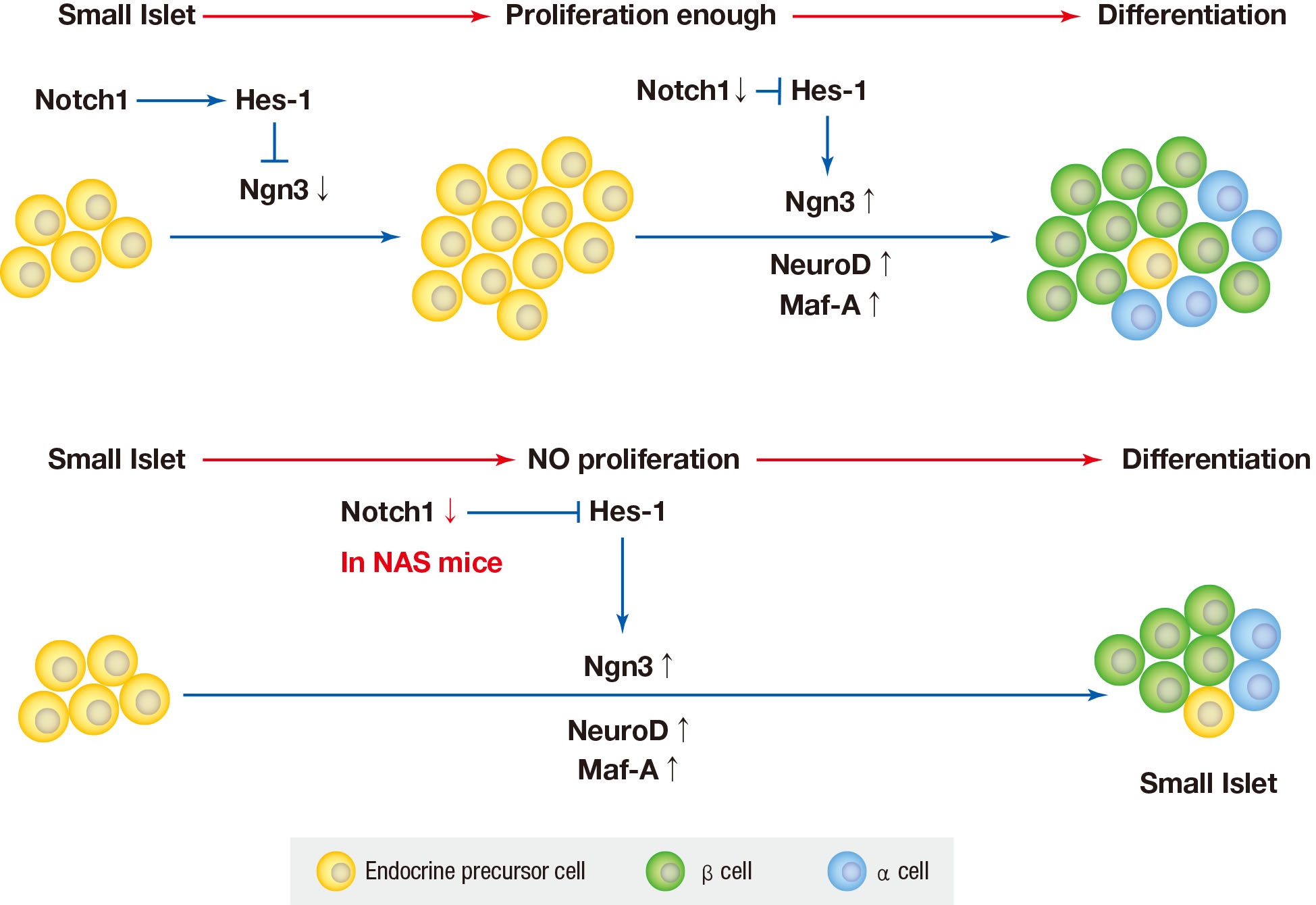
Background Notch signaling pathway plays an important role in regulating pancreatic endocrine and exocrine cell fate during pancreas development. Notch signaling is also expressed in adult pancreas. There are few studies on the effect of Notch on adult pancreas. Here, we investigated the role of Notch in islet mass and glucose homeostasis in adult pancreas using Notch1 antisense transgenic (NAS).
Methods Western blot analysis was performed for the liver of 8-week-old male NAS mice. We also conducted an intraperitoneal glucose tolerance test (IPGTT) and intraperitoneal insulin tolerance test in 8-week-old male NAS mice and male C57BL/6 mice (control). Morphologic observation of pancreatic islet and β-cell was conducted in two groups. Insulin secretion capacity in islets was measured by glucose-stimulated insulin secretion (GSIS) and perifusion.
Results NAS mice showed higher glucose levels and lower insulin secretion in IPGTT than the control mice. There was no significant difference in insulin resistance. Total islet and β-cell masses were decreased in NAS mice. The number of large islets (≥250 µm) decreased while that of small islets (<250 µm) increased. Reduced insulin secretion was observed in GSIS and perifusion. Neurogenin3, neurogenic differentiation, and MAF bZIP transcription factor A levels increased in NAS mice.
Conclusion Our study provides that Notch1 inhibition decreased insulin secretion and decreased islet and β-cell masses. It is thought that Notch1 inhibition suppresses islet proliferation and induces differentiation of small islets. In conclusion, Notch signaling pathway may play an important role in β-cell mass determination and diabetes.
-
Citations
Citations to this article as recorded by- N6-methylation of RNA-bound adenosine regulator HNRNPC promotes vascular endothelial dysfunction in type 2 diabetes mellitus by activating the PSEN1-mediated Notch pathway
Ying Cai, Tao Chen, Mingzhu Wang, Lihua Deng, Cui Li, Siqian Fu, Kangling Xie
Diabetes Research and Clinical Practice.2023; 197: 110261. CrossRef - Single‐cell RNA sequencing: Inhibited Notch2 signalling underlying the increased lens fibre cells differentiation in high myopia
Yunqian Yao, Ling Wei, Zhenhua Chen, Hao Li, Jiao Qi, Qingfeng Wu, Xingtao Zhou, Yi Lu, Xiangjia Zhu
Cell Proliferation.2023;[Epub] CrossRef - Micro ribonucleic acid‐363 regulates the phosphatidylinositol 3‐kinase/threonine protein kinase axis by targeting NOTCH1 and forkhead box C2, leading to hepatic glucose and lipids metabolism disorder in type 2 diabetes mellitus
Yu‐Huan Peng, Ping Wang, Xiao‐Qun He, Ming‐Zhao Hong, Feng Liu
Journal of Diabetes Investigation.2022; 13(2): 236. CrossRef - Soluble T-cadherin promotes pancreatic β-cell proliferation by upregulating Notch signaling
Tomonori Okita, Shunbun Kita, Shiro Fukuda, Keita Fukuoka, Emi Kawada-Horitani, Masahito Iioka, Yuto Nakamura, Yuya Fujishima, Hitoshi Nishizawa, Dan Kawamori, Taka-aki Matsuoka, Maeda Norikazu, Iichiro Shimomura
iScience.2022; 25(11): 105404. CrossRef - Comparison of islet isolation result and clinical applicability according to GMP‐grade collagenase enzyme blend in adult porcine islet isolation and culture
Kyungmin Kwak, Jae‐kyung Park, Joohyun Shim, Nayoung Ko, Hyoung‐Joo Kim, Yongjin Lee, Jun‐Hyeong Kim, Michael Alexander, Jonathan R. T. Lakey, Hyunil Kim, Kimyung Choi
Xenotransplantation.2021;[Epub] CrossRef - Genome-Wide Meta-analysis Identifies Genetic Variants Associated With Glycemic Response to Sulfonylureas
Adem Y. Dawed, Sook Wah Yee, Kaixin Zhou, Nienke van Leeuwen, Yanfei Zhang, Moneeza K. Siddiqui, Amy Etheridge, Federico Innocenti, Fei Xu, Josephine H. Li, Joline W. Beulens, Amber A. van der Heijden, Roderick C. Slieker, Yu-Chuan Chang, Josep M. Mercade
Diabetes Care.2021; 44(12): 2673. CrossRef
- N6-methylation of RNA-bound adenosine regulator HNRNPC promotes vascular endothelial dysfunction in type 2 diabetes mellitus by activating the PSEN1-mediated Notch pathway
- The Role of Glucagon-Like Peptide-1 Receptor Agonists in Type 2 Diabetes: Understanding How Data Can Inform Clinical Practice in Korea
- Seungjoon Oh, Suk Chon, Kyu Jeong Ahn, In-Kyung Jeong, Byung-Joon Kim, Jun Goo Kang
- Diabetes Metab J. 2015;39(3):177-187. Published online June 15, 2015
- DOI: https://doi.org/10.4093/dmj.2015.39.3.177
- 4,206 View
- 47 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Glucagon-like peptide-1 receptor agonists (GLP-1RAs) reduce glycosylated hemoglobin (HbA1c, 0.5% to 1.0%), and are associated with moderate weight loss and a relatively low risk of hypoglycemia. There are differences between Asian and non-Asian populations. We reviewed available data on GLP-1RAs, focusing on Korean patients, to better understand their risk/benefit profile and help inform local clinical practice. Control of postprandial hyperglycemia is important in Asians in whom the prevalence of post-challenge hyperglycemia is higher (vs. non-Asians). The weight lowering effects of GLP-1RAs are becoming more salient as the prevalence of overweight and obesity among Korean patients increases. The higher rate of gastrointestinal adverse events amongst Asian patients in clinical trials may be caused by higher drug exposure due to the lower body mass index of the participants (vs. non-Asian studies). Data on the durability of weight loss, clinically important health outcomes, safety and optimal dosing in Korean patients are lacking. Use of GLP-1RAs is appropriate in several patient groups, including patients whose HbA1c is uncontrolled, especially if this is due to postprandial glucose excursions and patients who are overweight or obese due to dietary problems (e.g., appetite control). The potential for gastrointestinal adverse events should be explained to patients at treatment initiation to facilitate the promotion of better compliance.
-
Citations
Citations to this article as recorded by- Tolerability and Effectiveness of Switching to Dulaglutide in Patients With Type 2 Diabetes Inadequately Controlled With Insulin Therapy
Youngsook Kim, Ji Hye Huh, Minyoung Lee, Eun Seok Kang, Bong-Soo Cha, Byung-Wan Lee
Frontiers in Endocrinology.2022;[Epub] CrossRef - Antihyperglycemic Agent Therapy for Adult Patients with Type 2 Diabetes Mellitus 2017: A Position Statement of the Korean Diabetes Association
Seung-Hyun Ko, Kyu-Yeon Hur, Sang Youl Rhee, Nan-Hee Kim, Min Kyong Moon, Seok-O Park, Byung-Wan Lee, Hyun Jin Kim, Kyung Mook Choi, Jin Hwa Kim
Diabetes & Metabolism Journal.2017; 41(5): 337. CrossRef - Antihyperglycemic agent therapy for adult patients with type 2 diabetes mellitus 2017: a position statement of the Korean Diabetes Association
Seung-Hyun Ko, Kyu-Yeon Hur, Sang Youl Rhee, Nan-Hee Kim, Min Kyong Moon, Seok-O Park, Byung-Wan Lee, Hyun Jin Kim, Kyung Mook Choi, Jin Hwa Kim
The Korean Journal of Internal Medicine.2017; 32(6): 947. CrossRef
- Tolerability and Effectiveness of Switching to Dulaglutide in Patients With Type 2 Diabetes Inadequately Controlled With Insulin Therapy
- Correlations between Glucagon Stimulated C-peptide Levels and Microvascular Complications in Type 2 Diabetes Patients
- Hye-Jin Yoon, Youn-Zoo Cho, Ji-young Kim, Byung-Joon Kim, Keun-Young Park, Gwan-Pyo Koh, Dae-Ho Lee, Dong-Mee Lim
- Diabetes Metab J. 2012;36(5):379-387. Published online October 18, 2012
- DOI: https://doi.org/10.4093/dmj.2012.36.5.379
- 5,907 View
- 43 Download
- 23 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background This study aimed to investigate whether stimulated C-peptide is associated with microvascular complications in type 2 diabetes mellitus (DM).
Methods A cross-sectional study was conducted in 192 type 2 diabetic patients. Plasma basal C-peptide and stimulated C-peptide were measured before and 6 minutes after intravenous injection of 1 mg glucagon. The relationship between C-peptide and microvascular complications was statistically analyzed.
Results In patients with retinopathy, basal C-peptide was 1.9±1.2 ng/mL, and stimulated C-peptide was 2.7±1.6 ng/mL; values were significantly lower compared with patients without retinopathy (
P =0.031 andP =0.002, respectively). In patients with nephropathy, basal C-peptide was 1.6±0.9 ng/mL, and stimulated C-peptide was 2.8±1.6 ng/mL; values were significantly lower than those recorded in patients without nephropathy (P =0.020 andP =0.026, respectively). Stimulated C-peptide level was associated with increased prevalence of microvascular complications. Age-, DM duration-, and hemoglobin A1c-adjusted odds ratios for retinopathy in stimulated C-peptide value were 4.18 (95% confidence interval [CI], 1.40 to 12.51) and 3.35 (95% CI, 1.09 to 10.25), respectively. The multiple regression analysis between nephropathy and C-peptide showed that stimulated C-peptide was statistically correlated with nephropathy (P =0.03).Conclusion In patients with type 2 diabetes, the glucagon stimulation test was a relatively simple method of short duration for stimulating C-peptide response. Stimulated C-peptide values were associated with microvascular complications to a greater extent than basal C-peptides.
-
Citations
Citations to this article as recorded by- A Nomogram for Predicting Vision-Threatening Diabetic Retinopathy Among Mild Diabetic Retinopathy Patients: A Case–Control and Prospective Study of Type 2 Diabetes
Jing Ke, Kun Li, Bin Cao
Diabetes, Metabolic Syndrome and Obesity.2023; Volume 16: 275. CrossRef - The average 30-minute post-prandial C-peptide predicted diabetic retinopathy progress: a retro-prospective study
Ting Pan, Jie Gao, Xinghua Cai, Huihui Zhang, Jun Lu, Tao Lei
BMC Endocrine Disorders.2023;[Epub] CrossRef - Dysregulation of miR-374a is involved in the progression of diabetic retinopathy and regulates the proliferation and migration of retinal microvascular endothelial cells
Zhanhong Wang, Xiao Zhang, Yanjun Wang, Dailing Xiao
Clinical and Experimental Optometry.2022; 105(3): 287. CrossRef - The Relationship between the Lipid Accumulation Product and Beta-cell Function in Korean Adults with or without Type 2 Diabetes Mellitus: The 2015 Korea National Health and Nutrition Examination Survey
Hye Eun Cho, Seung Bum Yang, Mi Young Gi, Ju Ae Cha, so Young Park, Hyun Yoon
Endocrine Research.2022; 47(2): 80. CrossRef - Effects of Serum C-Peptide Level on Blood Lipid and Cardiovascular and Cerebrovascular Injury in Patients with Type 2 Diabetes Mellitus: A Meta-Analysis
Juan Qin, Rongli Sun, Ding Ding, Yuvaraja Teekaraman
Contrast Media & Molecular Imaging.2022; 2022: 1. CrossRef - Investigation of Diabetes Complication Risk Perception and Diabetes Self-Management Skills in Individuals with Diabetes
Mehmet AYTEMUR, Bahar İNKAYA
Turkish Journal of Diabetes and Obesity.2022; 6(2): 121. CrossRef - Diabetic Retinopathy and Insulin Insufficiency: Beta Cell Replacement as a Strategy to Prevent Blindness
Eli Ipp
Frontiers in Endocrinology.2021;[Epub] CrossRef - Association of C-peptide with diabetic vascular complications in type 2 diabetes
Y. Wang, H. Wan, Y. Chen, F. Xia, W. Zhang, C. Wang, S. Fang, K. Zhang, Q. Li, N. Wang, Y. Lu
Diabetes & Metabolism.2020; 46(1): 33. CrossRef - Variations in glucose/C-peptide ratio in patients with type 2 diabetes associated with renal function
John A. D'Elia, Christopher Mulla, Jiankang Liu, Larry A. Weinrauch
Diabetes Research and Clinical Practice.2019; 150: 1. CrossRef - The pharmacokinetics of porcine C‐peptide after intraperitoneal injection
Naho Iizuka, Masuhiro Nishimura, Yasutaka Fujita, Osamu Sawamoto, Shinichi Matsumoto
Xenotransplantation.2019;[Epub] CrossRef - Association of KCNJ11(RS5219) gene polymorphism with biochemical markers of glycemic status and insulin resistance in gestational diabetes mellitus
Lenin M, Ramesh Ramasamy, Sweta Kulkarani, Seetesh Ghose, Srinivasan A.R.S., Sathish Babu M
Meta Gene.2018; 16: 134. CrossRef - Glucagon secretion is increased in patients with Type 2 diabetic nephropathy
Xiaoyu Wang, Juhong Yang, Baocheng Chang, Chunyan Shan, Yanguang Xu, Miaoyan Zheng, Ying Wang, Huizhu Ren, Liming Chen
Journal of Diabetes and its Complications.2016; 30(3): 488. CrossRef - Relationship between serum C-peptide level and diabetic retinopathy according to estimated glomerular filtration rate in patients with type 2 diabetes
Jin Ook Chung, Dong Hyeok Cho, Dong Jin Chung, Min Young Chung
Journal of Diabetes and its Complications.2015; 29(3): 350. CrossRef - Independent association between serum C‐peptide levels and fat mass‐to‐lean mass ratio in the aging process
Ying Li, Lian Shun Zheng, Yue Li, Duo Duo Zhao, Lu Meng
Geriatrics & Gerontology International.2015; 15(7): 918. CrossRef - Relationship Between β-Cell Function, Metabolic Control, and Microvascular Complications in Type 2 Diabetes Mellitus
Lihua Zhao, Jing Ma, Shaoxin Wang, Yun Xie
Diabetes Technology & Therapeutics.2015; 17(1): 29. CrossRef - Association of fasting insulin and C peptide with diabetic retinopathy in Latinos with type 2 diabetes
Jane Z Kuo, Xiuqing Guo, Ronald Klein, Barbara E Klein, Robert N Weinreb, Pauline Genter, Fone-Ching Hsiao, Mark O Goodarzi, Jerome I Rotter, Yii-Der Ida Chen, Eli Ipp
BMJ Open Diabetes Research & Care.2014; 2(1): e000027. CrossRef - Association between physical activity and serum C‐peptide levels among the elderly
Ying Li, Lu Meng, QianQian Miao, Yasuto Sato
Geriatrics & Gerontology International.2014; 14(3): 647. CrossRef - Age at Diagnosis and C-Peptide Level Are Associated with Diabetic Retinopathy in Chinese
Xiaoling Cai, Xueyao Han, Simin Zhang, Yingying Luo, Yingli Chen, Linong Ji, Alfred S. Lewin
PLoS ONE.2014; 9(3): e91174. CrossRef - Prevalence and risk factors for diabetic retinopathy in Asian Indians with young onset Type 1 and Type 2 Diabetes
Ramachandran Rajalakshmi, Anandakumar Amutha, Harish Ranjani, Mohammed K. Ali, Ranjit Unnikrishnan, Ranjit Mohan Anjana, K.M. Venkat Narayan, Viswanathan Mohan
Journal of Diabetes and its Complications.2014; 28(3): 291. CrossRef - Prediction of response to GLP-1 receptor agonist therapy in Japanese patients with type 2 diabetes
Kenjiro Imai, Tetsuro Tsujimoto, Atsushi Goto, Maki Goto, Miyako Kishimoto, Ritsuko Yamamoto-Honda, Hiroshi Noto, Hiroshi Kajio, Mitsuhiko Noda
Diabetology & Metabolic Syndrome.2014;[Epub] CrossRef - The Association between the Serum C-Peptide Level and Bone Mineral Density
Ying Li, Hua Liu, Yasuto Sato, Bin He
PLoS ONE.2013; 8(12): e83107. CrossRef - C-Peptide and Its Career from Innocent Bystander to Active Player in Diabetic Atherogenesis
Corinna Lebherz, Nikolaus Marx
Current Atherosclerosis Reports.2013;[Epub] CrossRef - C-Peptide and Vascular Complications in Type 2 Diabetic Subjects
Seok Man Son
Diabetes & Metabolism Journal.2012; 36(5): 345. CrossRef
- A Nomogram for Predicting Vision-Threatening Diabetic Retinopathy Among Mild Diabetic Retinopathy Patients: A Case–Control and Prospective Study of Type 2 Diabetes
- Response: Basal C-peptide Level as a Surrogate Marker of Subclinical Atherosclerosis in Type 2 Diabetic Patients (Diabetes Metab J 2011;35:41-9)
- Sung-Tae Kim, Byung-Joon Kim, Dong-Mee Lim, In-Geol Song, Jang-Han Jung, Kang-Woo Lee, Keun-Young Park, Youn-Zoo Cho, Dae-Ho Lee, Gwan-Pyo Koh
- Diabetes Metab J. 2011;35(2):190-191. Published online April 30, 2011
- DOI: https://doi.org/10.4093/dmj.2011.35.2.190
- 3,150 View
- 25 Download
- Basal C-peptide Level as a Surrogate Marker of Subclinical Atherosclerosis in Type 2 Diabetic Patients
- Sung-Tae Kim, Byung-Joon Kim, Dong-Mee Lim, In-Geol Song, Jang-Han Jung, Kang-Woo Lee, Keun-Young Park, Youn-Zoo Cho, Dae-Ho Lee, Gwan-Pyo Koh
- Diabetes Metab J. 2011;35(1):41-49. Published online February 28, 2011
- DOI: https://doi.org/10.4093/dmj.2011.35.1.41
- 4,040 View
- 37 Download
- 21 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Recent studies have revealed that C-peptide induces smooth muscle cell proliferation and causes human atherosclerotic lesions in diabetic patients. The present study was designed to examine whether the basal C-peptide levels correlate with cardiovascular risk in type 2 diabetes mellitus (T2DM) patients.
Methods Data was obtained from 467 patients with T2DM from two institutions who were followed for four years. The medical findings of all patients were reviewed, and patients with creatinine >1.4 mg/dL, any inflammation or infection, hepatitis, or type 1 DM were excluded. The relationships between basal C-peptide and other clinical values were statistically analyzed.
Results A simple correlation was found between basal C-peptide and components of metabolic syndrome (MS). Statistically basal C-peptide levels were significantly higher than the three different MS criteria used in the present study, the Adult Treatment Panel III (ATP III) of the National Cholesterol Education Program's (NCEP's), World Health Organization (WHO), and the International Diabetes Federation (IDF) criteria (NCEP-ATP III,
P =0.001; IDF,P <0.001; WHO,P =0.029). The multiple regression analysis between intima-media thickness (IMT) and clinical values showed that basal C-peptide significantly correlated with IMT (P =0.043), while the analysis between the 10-year coronary heart disease risk by the United Kingdom Prospective Diabetes Study risk engine and clinical values showed that basal C-peptide did not correlate with IMT (P =0.226).Conclusion Basal C-peptide is related to cardiovascular predictors (IMT) of T2DM, suggesting that basal C-peptide does provide a further indication of cardiovascular disease.
-
Citations
Citations to this article as recorded by- The Correlation Between C-Peptide and Severity of Peripheral Atherosclerosis in Type 2 Diabetes Mellitus
Maisa A Wahab, Alshaymaa Alhabibi, Ahmed Khairy Sakr, Mohamed Yahia Zakaria, Ola I Saleh, Inass Hassan Ahmad, Eman Abdelrahman, Randa Taha, Fayka Karem Abdel Azeem Ahmed, Bothayna Ismail, Lamiaa Hosney Azel, Asmaa S Hassan, Hanaa Mohammed Eid El Sayed, Sa
Diabetes, Metabolic Syndrome and Obesity.2023; Volume 16: 2617. CrossRef - Blood C‐peptide concentration as a proxy marker of cardiovascular disease: An observational cross‐sectional study
Laurinda Adusu‐Donkor, Emmanuel Kwaku Ofori, Fleischer C. N. Kotey, Francis Kwaku Dogodzi, Wormenor Dziedzorm, Alfred Buabeng, Segla Kwame Bernard, Seth K. Amponsah, Henry Asare‐Anane
Health Science Reports.2023;[Epub] CrossRef - The impact of insulin induced lipohypertrophy on carotid intima-media thickness in patients with type 2 diabetes mellitus
Cem Onur Kirac, Vehbi Sirikci, Huseyin Avni Findikli
Medicine.2023; 102(39): e34696. CrossRef - Effects of Serum C-Peptide Level on Blood Lipid and Cardiovascular and Cerebrovascular Injury in Patients with Type 2 Diabetes Mellitus: A Meta-Analysis
Juan Qin, Rongli Sun, Ding Ding, Yuvaraja Teekaraman
Contrast Media & Molecular Imaging.2022; 2022: 1. CrossRef - Correlation between serum C-peptide-releasing effects and the risk of elevated uric acid in type 2 diabetes mellitus
Yanyan Liu, Xue Zhao, Zequn Yang, Shurui Wang, Cong Han, Huijuan Zhang
Endocrine Journal.2022; 69(7): 773. CrossRef - Human C-peptide is a ligand of the elastin-receptor-complex and therewith central to human vascular remodelling and disease in metabolic syndrome
Gert Wensvoort
Medical Hypotheses.2022; 168: 110964. CrossRef - Influence of blood glucose fluctuation, C-peptide level and conventional risk factors on carotid artery intima–media thickness in Chinese Han patients with type 2 diabetes mellitus
Min Liu, Li Ao, Xinyu Hu, Jianning Ma, Kena Bao, Ye Gu, Jing Zhao, Weiping Huang
European Journal of Medical Research.2019;[Epub] CrossRef - Serum C peptide and carotid intima-medial thickness are independent markers of glucose intolerance among patients with ischemic cerebrovascular stroke
Nearmeen M. Rashad, Ghada M. Samir, Hanan M. Sabry, Nesreen M. Mohy, Shereen M. El Shabrawy
The Egyptian Journal of Internal Medicine.2019; 31(3): 368. CrossRef - Biomarker potential of C-peptide for screening of insulin resistance in diabetic and non-diabetic individuals
Haseeb A. Khan, Samia H. Sobki, Aishah Ekhzaimy, Isra Khan, Mona A. Almusawi
Saudi Journal of Biological Sciences.2018; 25(8): 1729. CrossRef - SERUM C-PEPTIDE LEVEL IN OBESE AND NON-OBESE PATIENTS WITH TYPE 2 DIABETES MELLITUS
Shamha Beegum Mariyam, Saboora Beegum Muthubeevi, Sandhya Chandrasekharan Vasantha
Journal of Evolution of Medical and Dental Sciences.2017; 6(05): 350. CrossRef - Mechanisms of action and therapeutic potential of proinsulin C-peptide
A. O. Shpakov
Journal of Evolutionary Biochemistry and Physiology.2017; 53(3): 180. CrossRef - Hemolysis Affects C‐Peptide Immunoassay
Zhi‐Qi Wu, Ju Lu, Hua‐Guo Xu
Journal of Clinical Laboratory Analysis.2016; 30(6): 1232. CrossRef - Lipid and inflammatory biomarker profiles in early insulin resistance
Itahisa Marcelino Rodríguez, José Oliva García, José Juan Alemán Sánchez, Delia Almeida González, Santiago Domínguez Coello, Buenaventura Brito Díaz, Fadoua Gannar, María del Cristo Rodríguez Pérez, Roberto Elosua, Antonio Cabrera de León
Acta Diabetologica.2016; 53(6): 905. CrossRef - C-Peptide Is Independently Associated with an Increased Risk of Coronary Artery Disease in T2DM Subjects: A Cross-Sectional Study
Lingshu Wang, Peng Lin, Aixia Ma, Huizhen Zheng, Kexin Wang, Wenjuan Li, Chuan Wang, Ruxing Zhao, Kai Liang, Fuqiang Liu, Xinguo Hou, Jun Song, Yiran Lu, Ping Zhu, Yu Sun, Li Chen, Marta Letizia Hribal
PLOS ONE.2015; 10(6): e0127112. CrossRef - C-peptide as a risk factor of coronary artery disease in the general population
Antonio Cabrera de León, José Gregorio Oliva García, Itahisa Marcelino Rodríguez, Delia Almeida González, José Juan Alemán Sánchez, Buenaventura Brito Díaz, Santiago Domínguez Coello, Vicente Bertomeu Martínez, Armando Aguirre Jaime, María del Cristo Rodr
Diabetes and Vascular Disease Research.2015; 12(3): 199. CrossRef - Gender differences in the association of insulin resistance and high-sensitivity c-reactive protein in obese adolescents
Ramin Alemzadeh, Jessica Kichler
Journal of Diabetes & Metabolic Disorders.2014;[Epub] CrossRef - Cytokinome Profile of Patients with Type 2 Diabetes and/or Chronic Hepatitis C Infection
Susan Costantini, Francesca Capone, Eliana Guerriero, Raffaele Marfella, Angela Sorice, Patrizia Maio, Michele Di Stasio, Giuseppe Paolisso, Giuseppe Castello, Giovanni Colonna, Patricia Fitzgerald-Bocarsly
PLoS ONE.2012; 7(6): e39486. CrossRef - Serum glycated albumin predicts the progression of carotid arterial atherosclerosis
Sun Ok Song, Kwang Joon Kim, Byung-Wan Lee, Eun Seok Kang, Bong Soo Cha, Hyun Chul Lee
Atherosclerosis.2012; 225(2): 450. CrossRef - C-Peptide: A New Mediator of Atherosclerosis in Diabetes
Dusica Vasic, Daniel Walcher
Mediators of Inflammation.2012; 2012: 1. CrossRef - Letter: Basal C-peptide Level as a Surrogate Marker of Subclinical Atherosclerosis in Type 2 Diabetes Patients (Diabetes Metab J 2011;35:41-9)
Min Suk Lee, Hae Jin Kim
Diabetes & Metabolism Journal.2011; 35(2): 188. CrossRef - Response: Basal C-peptide Level as a Surrogate Marker of Subclinical Atherosclerosis in Type 2 Diabetic Patients (Diabetes Metab J 2011;35:41-9)
Sung-Tae Kim, Byung-Joon Kim, Dong-Mee Lim, In-Geol Song, Jang-Han Jung, Kang-Woo Lee, Keun-Young Park, Youn-Zoo Cho, Dae-Ho Lee, Gwan-Pyo Koh
Diabetes & Metabolism Journal.2011; 35(2): 190. CrossRef
- The Correlation Between C-Peptide and Severity of Peripheral Atherosclerosis in Type 2 Diabetes Mellitus
- Correlations of Glucose Levels in Interstitial Fluid Estimated by Continuous Glucose Monitoring Systems and Venous Plasma
- Byung-Joon Kim
- Korean Diabetes J. 2010;34(6):338-339. Published online December 31, 2010
- DOI: https://doi.org/10.4093/kdj.2010.34.6.338
- 2,675 View
- 36 Download

 KDA
KDA
 First
First Prev
Prev





